Dr. Friedman's Office: (210) 222-2154
Age Related Macular Degeneration
“Age-related macular degeneration (AMD) is the number one leading cause of blindness in adults over 65 in the developed world.” That is a common introduction to this disease in many articles, but what does that mean? Although it sounds ominous and severe, ARMD has many features, and the spectrum of disease can be mild to severe. Herein, let me try and boil down the high-points of this disease as I usually explain it to patients.
Throughout our life, our eyes (much like the rest of our body) are constantly being exposed to the environment. The retina (which is the part of the eye responsible for taking the world we see and sending that picture to the brain) is particularly exposed to a lot of environmental stressors. Due to smoking, an unhealthy diet, sun exposure, or any number of reasons, our organs build up waste products. Our retinas are no different. Much like you can get hard arteries and heart diseases from too much unhealthy food throughout life, our retinas sometimes build up too much waste. These waste products can clump together underneath the retina and form deposits called drusen. The macula (which is the part of the retina corresponding to the central part of your vision) tends to collect these deposits.
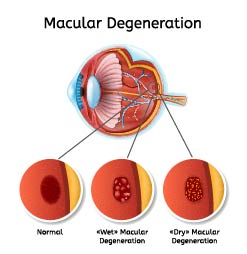
Drusen are the start of age-related macular degeneration and if you have enough of them in your eyes, you have a diagnosis of “dry” age-related macular degeneration. There are more specific ways of classifying these drusen (e.g., soft, hard, small, medium, large, etc.), but for now, what you need to remember is drusen = macular degeneration. People with drusen in their eyes rarely experience problems with their central vision. They might notice some loss of contrast or reading trouble with small print, but the overall vision remains relatively good.
The problem is that these waste deposits set up an environment under the retina that can allow progression to “wet” macular degeneration. Ninety-percent (90%) of people with macular degeneration have the dry form. That means only 10% of people with ARMD progress to wet macular degeneration. Wet macular degeneration is the more devastating type of disease. In this form of the disease, new blood vessels form in and under the retina; these vessels can leak and break causing a significant loss of vision. Blood or other fluid can cause the layers of the retina to separate which causes distortion and loss of vision centrally.
There is also another means of losing vision in ARMD known as geographic atrophy. It is important to remember that ARMD is a “degenerative” disease. The support cells underneath the retina that keep it alive and healthy are slowly dying. If these support cells are completely gone, the receptors that process light and allow us to see (photoreceptors) can no longer work, and we lose vision. That is the essence of geographic atrophy.
Here are a couple of things to remember about macular degeneration. First, it is a slowly progressive disease in most instances. If you have macular degeneration and you experience a sudden change in your central vision, then that is an indication that you should probably be seen by your ophthalmologist in the near future to ensure that you have not converted to “wet” macular degeneration. Also, macular degeneration is appropriately named because it affects the center of your vision (the macula). If you notice that you are missing your peripheral vision (side vision), then you need to be evaluated for another cause of this vision loss. Finally, macular degeneration does not cause you to go completely, “lights-out”, blind. Although it can cause significant loss of central vision and the ability to make out detail, complete vision loss in one or both eyes is an indication that something else is at work.
So what can be done for macular degeneration?
First, if you have dry macular degeneration, the goal is to slow down the rate of visual loss and prevent conversion to wet macular degeneration. There is a lot of ongoing research to try and tackle both of these efforts and there are several steps you can take. The best medicinal means of treatment we have right now are eye vitamins that adhere to the AREDS 2 guidelines. Although I could delve into all the details, I posted a blog about the changes in the eye vitamin world, so head on over to the News/Blog page to read up on that. In short, you should only be using these vitamins if you have moderate to severe dry macular degeneration (a recommendation to be made by your eye care specialist). Also, I recommend some healthy lifestyle choices as macular degeneration is caused by inflammation and waste deposits in the retina. All of those good anti-oxidants that you get from leafy green vegetables, whole grains, exercise, etc. can actually help your eyes. I will spend a later post on good dietary choices for the eyes, so stay tuned. Finally, if you smoke, QUIT!!! There have been plenty of good studies showing a link between worsening age-related macular degeneration and smoking. If loss of vision isn’t a convincing argument for quitting smoking, I don’t know what is.

Wet macular degeneration is a different entity. Those leaking blood vessels need to be stopped. Up until about a decade ago, all we could do was watch as the retina bled and formed a scar that left patients with permanent and substantial visual loss. Some physicians tried using special laser therapy to close off leaky blood vessels, and although this treatment worked, there is now a better therapy. The blood vessels that cause all of the trouble in the back of the eye are regulated by a messenger in the eye known as vascular endothelial growth factor (VEGF). Fortunately, we now have many medications that can actually bind this messenger (anti-VEGF) and keep it from telling the retina to make leaky vessels. The three main treatments available are (in alphabetical order by brand name): Avastin, Eylea, and Lucentis. I could put the generic names out there, but they are long and cause a lot of confusion because they sound alike. There will be a new section soon about the differences between these medications and all of the controversy surrounding them, but the point remains that we have medications that can fight progression of wet age related macular degeneration.
A Brief Aside
Whenever I mention any of these intravitreal medications, we have to have “the talk”. Yes, intravitreal means that the medicine goes directly into the eye. Before you go running the other direction and click away from the webpage, bear in mind that across the nation there are thousands of ophthalmologists doing these sorts of injections many times a day. As I stated at the beginning, ARMD is the leading cause of visual loss in people over 65 years old. Obviously, you don’t see a lot of 65+ people walking around with their hands over their eyes on a day-to-day basis. The injection is done with a very small needle and the eye is numbed beforehand with good medicine to make sure that there is minimal discomfort. The eye is also cleaned with antibacterial soap to try and ensure no infection occurs after the injection. I cannot guarantee that you won’t feel it when a small needle goes into the eye. Most patients complain about a surprising, pressure sensation, but not pain.
I also want to take a moment to caution anybody that is receiving these medications. Most of the time, eye injections go off without a hitch, but every so often (anywhere from 1-in-2000 to 1-in-5000 injections) the eye can get an infection inside it. This is known as endophthalmitis, and it can have serious consequences if not treated promptly. If after receiving an injection in the eye, you notice that the vision starts to get a lot worse and the eye starts to get really painful, DO NOT shrug it off. Have an eye doctor check you immediately because if it is an infection, it needs to be treated with antibiotics or even surgery.
(Also, do not eat or drink anything before going to see the doctor if you have a painful eye because if they have to take you to surgery, you need to have an empty stomach for about 6-8 hours.) Again, this is a rare complication, but it can happen, so be aware.
Back to the story of ARMD . . .
Now that we have gotten past the scary part, back to the treatment. There are a couple of things to keep in mind. First, the medicine wears off. Just like any other medication that you take by mouth, your body uses up the medicine that is put in the eye. When it runs out, you have to replace it. Usually, this takes about a month, but some people use it faster and some people use it slower. When the medicine runs out, the blood vessels can start to leak again and cause vision loss. In fact, the blood vessels in wet macular degeneration never really go away (although researchers are working on medications that can make that possible). You might be visiting your ophthalmologist on a pretty regular basis to ensure that you always have enough anti-VEGF medicine in your eyes. Still, the outcomes are good. People who developed wet macular degeneration and lost vision were able to gain back at least 3 lines of vision (if not more) on a standard eye chart if they were treated with these medications more often than people not treated with the medicine. This has been substantiated in numerous studies. Again, it does not work for everybody, but these injections are probably the best treatment we currently have available.
Macular degeneration can be a devastating disease if it is not monitored and treated appropriately, but with regular checks, the loss of vision should be slow and manageable. Please feel free to contact us with any more specific questions about macular degeneration as it is a disease that requires a lot of explanation. I hope this summary gives a little insight into the basics of the disease.
Duncan Friedman
Retina Specialist
San Antonio, Texas